Sulfa drugs, especially Bactrim (sulfamethoxazole/trimethoprim), are widely prescribed antibiotics used to treat common infections such as urinary tract infections (UTIs), respiratory infections, and skin conditions. Despite their effectiveness, sulfa medications frequently cause skin reactions—commonly referred to as a “Bactrim rash” or “Sulfa drug rash.” While most sulfa rashes are mild and easily managed, some reactions can become serious or even life-threatening, such as Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN).
This guide (updated in 2025) clearly outlines what you need to know about recognizing sulfa drug rashes, distinguishing mild from severe symptoms, and managing potential allergic reactions effectively.
Understanding Sulfa Drug Rash (Bactrim Rash)
What Causes Sulfa Drug Rash?
Sulfa drugs belong to a class of antibiotics known as sulfonamides. The rash associated with these antibiotics is usually caused by an immune-mediated allergic response. The body’s immune system mistakenly identifies the sulfa medication as a harmful substance, releasing histamines and other inflammatory mediators that trigger a skin rash.
Bactrim, specifically, is a combination of sulfamethoxazole and trimethoprim. Sulfamethoxazole is responsible for the allergic reaction in sensitive individuals.
Common Symptoms of Sulfa Drug Rash
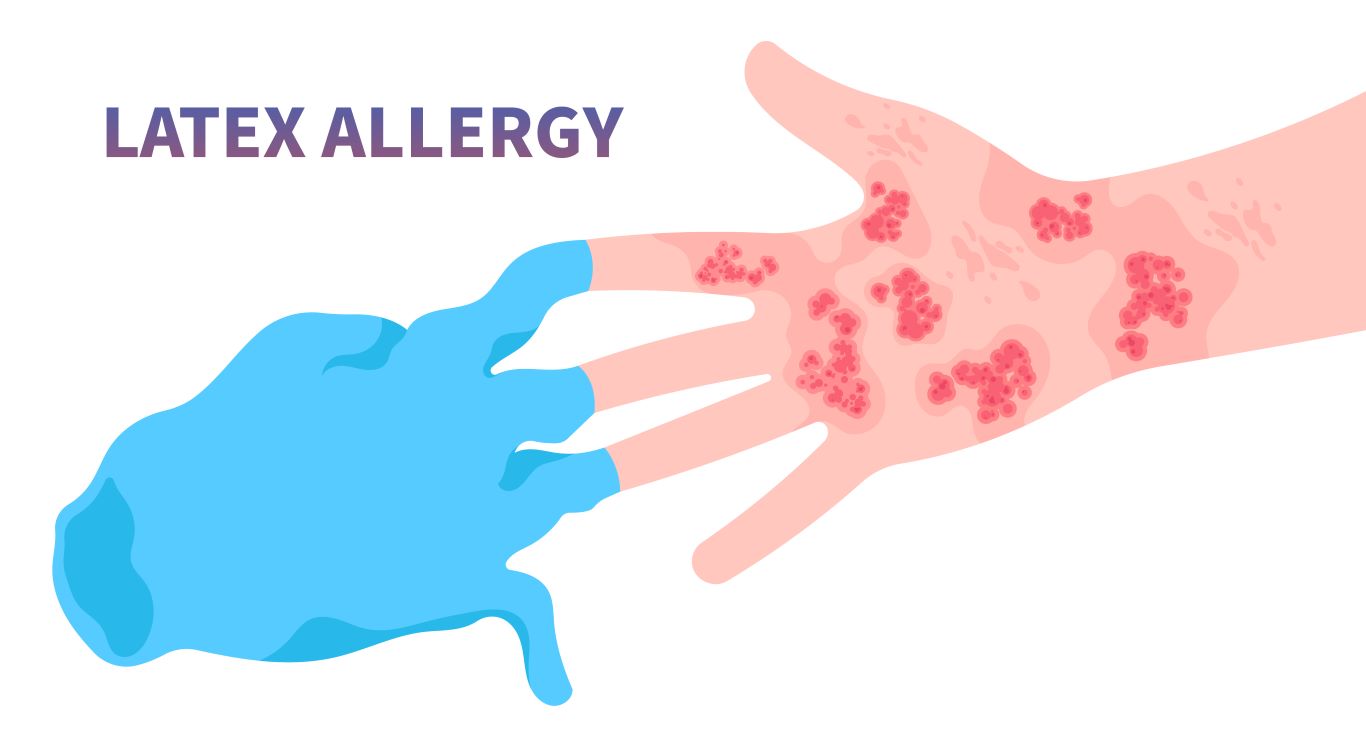
Sulfa drug rash commonly manifests as:
- Maculopapular rash: red, flat patches combined with raised bumps.
- Urticaria (Hives): itchy, raised red welts.
- Generalized itching or redness without specific rash formations.
According to recent studies (JAMA Dermatology, 2024), about 3% to 8% of patients prescribed sulfa antibiotics like Bactrim develop a rash, most of which are mild and self-limited.
Mild vs Severe Reactions: When to Worry?
Mild Symptoms (Usually Harmless):
- Slight redness or pinkish rash, typically appearing within days after starting treatment.
- Mild itching or discomfort.
- Usually resolves spontaneously after discontinuing the medication.
If you experience mild symptoms without additional signs like fever or blisters, consult your doctor about potentially discontinuing Bactrim under supervision.
Severe Symptoms (Require Immediate Medical Attention):
Serious allergic reactions to sulfa drugs can escalate quickly. Watch for:
- Blistering or peeling skin: This could indicate Stevens-Johnson syndrome or Toxic Epidermal Necrolysis.
- Fever, chills, or joint pain: Systemic symptoms suggest a more severe reaction.
- Mucosal involvement: Mouth sores, red or swollen eyes, or genital lesions often indicate severe reactions.
- Facial swelling, breathing difficulties, dizziness: These are signs of anaphylaxis, a severe allergic reaction requiring emergency medical attention.
A 2025 update from the American Academy of Allergy, Asthma & Immunology (AAAAI) indicates that approximately 0.5% of sulfa-drug rashes can progress into life-threatening conditions like SJS or TEN, highlighting the importance of immediate intervention.
Recognizing Stevens-Johnson Syndrome (SJS)
What is Stevens-Johnson Syndrome?
Stevens-Johnson syndrome is a rare, severe allergic reaction affecting the skin and mucous membranes, characterized by blistering, peeling, and painful skin lesions. This potentially life-threatening condition is strongly associated with sulfa antibiotics, NSAIDs, and anticonvulsants.
Critical Signs of SJS:
- Severe rash rapidly progressing into painful blisters.
- Mucosal sores (mouth, throat, eyes, genital area).
- Fever, flu-like symptoms, body aches.
- Significant pain or discomfort.
- Skin peeling, resembling severe burns.
If any of these symptoms occur after taking sulfa medications, seek immediate medical assistance.
A study published in the New England Journal of Medicine (2023) reinforced the necessity of early recognition and intervention, significantly reducing mortality and complications.
Diagnosis and Treatment of Sulfa Drug Rash
How is Sulfa Allergy Diagnosed?
Diagnosing sulfa allergies typically involves:
- Detailed patient history and physical examination.
- Skin allergy tests or controlled oral challenges (performed by an allergist) in uncertain cases.
Recent 2025 guidelines from the American College of Allergy, Asthma & Immunology (ACAAI) emphasize allergy verification to prevent unnecessary avoidance of beneficial antibiotics.
Management and Treatment Strategies:
- Immediate discontinuation of the medication: Stopping the sulfa antibiotic promptly under medical supervision is critical.
- Antihistamines: Medications such as diphenhydramine (Benadryl) or cetirizine (Zyrtec) can relieve itching and mild allergic symptoms.
- Topical Steroids: Hydrocortisone creams may reduce inflammation and itching for mild-to-moderate rashes.
- Systemic Steroids and supportive care: In severe cases (like SJS), hospital admission, corticosteroids, intravenous fluids, and supportive skin care become mandatory.
Safe Alternatives to Sulfa Drugs (If Allergic)
Patients allergic to sulfa antibiotics should inform all healthcare providers to avoid accidental exposure. Safe antibiotic alternatives include:
- Nitrofurantoin (Macrobid): Often prescribed for urinary tract infections as a sulfa-free alternative.
- Cephalosporins (e.g., cephalexin): Generally safe but check with an allergist if a severe sulfa allergy exists.
- Amoxicillin or Penicillin-based Antibiotics: Safe options for bacterial respiratory infections unless also allergic to penicillin.
- Doxycycline: Useful for skin and respiratory infections, providing a non-sulfa, non-penicillin alternative.
The latest 2025 Infectious Diseases Society of America (IDSA) recommendations stress personalized antibiotic selection after confirming sulfa allergy.
Long-term Considerations and Preventive Measures
Long-term Implications of Sulfa Allergy:
Once a sulfa drug allergy is confirmed, it usually remains lifelong. Documenting your allergy clearly on medical records and pharmacy files is essential. A verified sulfa allergy may also slightly increase the risk of reactions to other medications such as:
- Sulfasalazine (used for inflammatory bowel disease or rheumatoid arthritis).
- Diuretics like hydrochlorothiazide or furosemide (Lasix), which share sulfa chemical structures.
Discuss alternative options with your healthcare provider to minimize risk.
Prevention and Preparedness Tips:
- Inform healthcare professionals: Always mention your sulfa allergy during medical consultations.
- Wear medical alert bracelets: Useful during emergencies if you’re unable to communicate your allergy.
- Educate yourself: Know common medications that contain sulfa groups and always check labels.
FAQ: Sulfa Drug Rash Quick Reference
Q: Is a Bactrim rash always dangerous?
A: Not always. Most Bactrim rashes are mild, but severe signs like blistering or mucosal involvement need urgent attention.
Q: How long does a sulfa rash last?
A: Mild rashes typically resolve within days after stopping medication. Severe reactions require medical intervention and may take weeks to heal.
Q: Can I take other antibiotics after a sulfa rash?
A: Yes, several antibiotics like nitrofurantoin, doxycycline, or certain cephalosporins are generally safe after a sulfa allergy diagnosis.
Summary & Key Takeaways:
- Sulfa drug rash (Bactrim rash) commonly occurs due to allergic reactions to sulfamethoxazole.
- Symptoms range from mild irritation to severe life-threatening conditions (SJS or TEN).
- Recognizing severe symptoms (blisters, mucosal sores, fever) is crucial for timely medical intervention.
- Diagnosis involves careful clinical evaluation, sometimes allergy testing.
- Alternatives to sulfa drugs exist; document and communicate your allergy to healthcare providers clearly.
Reliable References (2025):
Infectious Diseases Society of America (IDSA) guidelines on antibiotic alternatives (2025). www.idsociety.org
American Academy of Allergy, Asthma & Immunology (AAAAI). www.aaaai.org
New England Journal of Medicine. Stevens-Johnson syndrome management (2023). www.nejm.org
American College of Allergy, Asthma & Immunology (ACAAI). Allergy testing guidelines (2025). acaai.org
This article reviewed by Dr. Jim Liu, MD.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc #menopause #hormone replacement