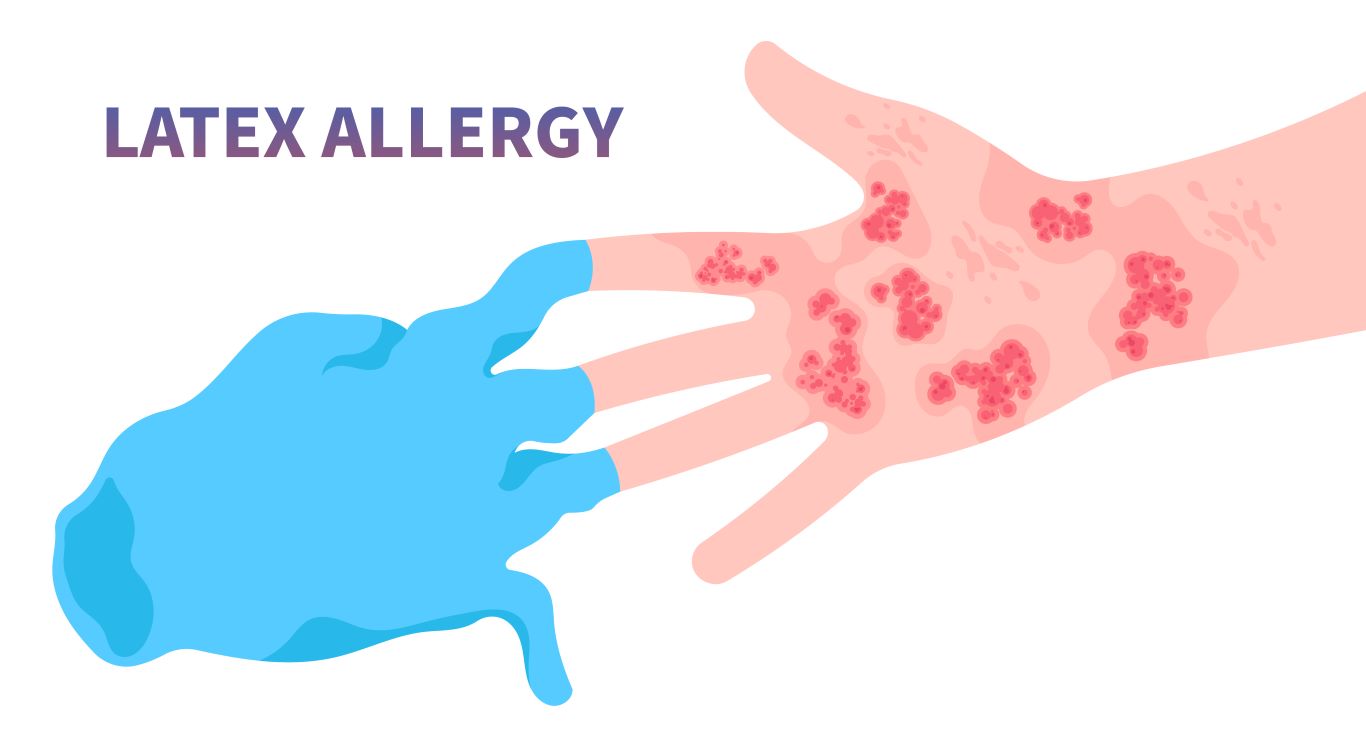
Latex, a natural rubber product, is ubiquitous in our daily lives—from medical gloves and bandages to balloons and even some clothing. While incredibly useful, for many, exposure to latex can trigger an allergic reaction, ranging from mild skin irritation to severe, life-threatening responses. Understanding a latex allergy is crucial for management, and thankfully, modern telehealth consultations offer a convenient and efficient way to get diagnosed and receive guidance.
This guide (updated for 2025) clearly outlines what you need to know about recognizing latex allergy symptoms, managing exposure, and how telehealth can streamline your path to diagnosis and effective management.
Understanding Latex Allergies
What is a Latex Allergy?
A latex allergy is an allergic reaction to proteins found in natural rubber latex. It’s an immune system response where the body mistakenly identifies these latex proteins as harmful invaders. Repeated exposure to latex products can increase the risk of developing this allergy. Healthcare workers, individuals with spina bifida, and those with other allergies (especially to certain foods like avocado, banana, kiwi, chestnut, or passion fruit – known as latex-fruit syndrome) are at higher risk.
Types of Reactions and Common Symptoms:
- Irritant Contact Dermatitis: This is the least severe reaction and is not a true allergy. It’s caused by irritation from chemical additives in latex gloves or from repeated hand washing, not the latex proteins themselves. Symptoms include dry, itchy, irritated, and sometimes cracked skin, usually on the hands.
- Allergic Contact Dermatitis (Delayed Hypersensitivity): This is a true, but delayed, allergic reaction, often resembling poison ivy. It’s caused by chemicals used in processing latex. Symptoms include a red, itchy rash, blisters, and crusting, appearing 12-48 hours after contact.
- Immediate Hypersensitivity (Type I Allergy): This is the most serious type of latex allergy and can be life-threatening. It’s an immediate reaction to the latex proteins themselves. Symptoms typically appear within minutes of exposure and can include:
- Skin: Hives (urticaria), redness, itching, swelling.
- Respiratory: Runny nose, sneezing, itchy eyes, scratchy throat, asthma symptoms (wheezing, difficulty breathing, chest tightness).
- Systemic: Rapid heart rate, dizziness, nausea, vomiting, abdominal cramps, low blood pressure, and anaphylaxis (a severe, whole-body allergic reaction involving widespread swelling, severe breathing difficulties, and a sudden drop in blood pressure, requiring immediate emergency medical attention).
Diagnosis and Management Through Telehealth
How Telehealth Can Help with Latex Allergy Diagnosis:
Traditionally, diagnosing a latex allergy involved in-person visits to an allergist. However, telehealth has revolutionized accessibility:
- Initial Consultation: You can schedule a virtual consultation with an allergist or your primary care provider. They can take a detailed medical history, discuss your symptoms, and assess your risk factors.
- Symptom Review: You can describe your reactions, when they occur, and what latex products you suspect. You might even be able to show skin reactions via video.
- Guidance for Testing: While definitive diagnostic tests (like blood tests for latex-specific IgE antibodies or skin prick tests, which should only be performed under strict medical supervision due to anaphylaxis risk) typically require an in-person visit, your telehealth provider can order these tests and guide you on where to get them done safely.
- Results Interpretation: Once results are available, your doctor can review them with you virtually, explain the diagnosis, and discuss next steps.
A 2025 report from the American Telemedicine Association (ATA) emphasizes the growing role of telehealth in allergy and immunology, especially for initial screenings and follow-up care, reducing the need for multiple in-person visits.
Management and Treatment Strategies:
- Strict Avoidance: This is the cornerstone of managing a latex allergy. Carefully read labels, inform healthcare providers, and choose latex-free alternatives for gloves, bandages, and other products.
- Medication for Mild Symptoms:
- Antihistamines: OTC antihistamines can help manage mild skin itching and hives.
- Topical Steroids: For contact dermatitis, a doctor might recommend a topical corticosteroid cream.
- Emergency Preparedness (for Type I Allergy):
- Epinephrine Auto-Injector: If you have a severe latex allergy, your doctor will likely prescribe an epinephrine auto-injector (e.g., EpiPen). You must carry it at all times and know how to use it.
- Medical Alert Identification: Wearing a medical alert bracelet or necklace can inform others of your allergy in an emergency.
- Action Plan: Your allergist will help you develop an anaphylaxis action plan.
Long-term Considerations and Prevention
Prevention Tips:
- Educate Yourself: Know common products containing latex.
- Inform Others: Tell family, friends, colleagues, and all healthcare providers about your allergy.
- Be Proactive: Request latex-free environments in healthcare settings.
Living with a latex allergy requires vigilance, but with proper diagnosis and management, you can significantly reduce your risk of exposure and adverse reactions. Telehealth provides an invaluable tool in this process, making expert care more accessible than ever.
Conclusions and Key Takeaways:
- Latex allergy is an immune reaction to proteins in natural rubber, with symptoms ranging from mild skin irritation to severe anaphylaxis.
- Identifying the type of reaction (irritant, allergic contact, or immediate hypersensitivity) is crucial for proper management.
- Telehealth offers a convenient way to consult with healthcare providers for diagnosis, testing guidance, and results interpretation.
- Strict avoidance of latex products is the primary management strategy.
- For severe allergies, carrying an epinephrine auto-injector and having an action plan are vital.
Trusted References (2025):
- American Academy of Allergy, Asthma & Immunology (AAAAI). www.aaaai.org
- American College of Allergy, Asthma & Immunology (ACAAI). acaai.org
- American Telemedicine Association (ATA). www.americantelemed.org (Refer to 2025 publications on allergy and immunology.)
This article reviewed by Dr. Jim Liu, MD.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc #menopause #hormone replacement